

Previous
Next
Our Goal
We at the Health Within Reach Foundation are committed "to revolutionize healthcare by making it Universally Accessible, Inclusive and Affordable for All.
Problem we are trying to solve
- 69% of population of India lives in Rural areas and lacks disproportionately in required number of healthcare professionals and infrastructure. (Census 2011)
- 26% of Urban population can not avail quality Health care services due to the financial barriers. (Rangarajan Report)
- So in total, approx. 75% of population in India faces at least one access barrier to healthcare.
- 31% of the population has to travel more than 30 kms to seek healthcare in rural India.
The situation is worse in Dental services across India.
- There is hardly one dentist for 2 Lakh population in rural India (WHO recommends 1:7,500).
- Untreated dental caries (tooth decay) in permanent teeth is the most common health condition according to the Global Burden of Disease 2019.
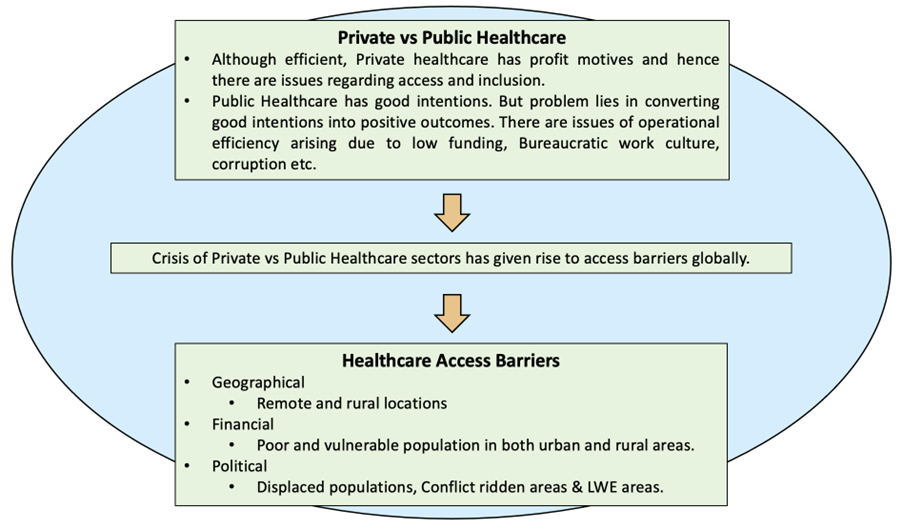
With due respect to current operating model of Healthcare delivery, there are serious concerns of inclusion and universal access to quality healthcare. This might result in missing our Sustainable Development Goal (SDG – 3) of “Health for All”.
Solution We Offer
A movable, Tech enabled self-contained health care unit (in a vehicle) within or from which intended health care services are provided to individuals.
Features –
- Hybrid – Polyclinic
- Model Van will consist of MBBS doctor & Dentist
- Technology enabled
- Fully Digital, paperless operations
- Telemedicine
- Digitally equipped referrals with complete handholding
- Operational efficiency through Workforce and Fleet management softwares
- Advanced Diagnostic services like ECG, Hb, HbA1C – in the mobile van itself.
- Long term goal of integration with existing healthcare setup
Why Mobile Clinics
- Cost :
- The return on investment of the Family Van was estimated at $1:$30 based on prevention services provided and ED visits avoided (Oriol et al BMC Central 2009).
- $1:$12 Saving for National Economy (Mobile Heath Map Harvard University)
- Healthcare Quality:
- Visiting the Family Van was associated with reductions in blood pressure by amounts correlated to a 30% relative risk reduction of heart attack and 40% relative risk of stroke (Song, Hill et al Health Affairs 2012).
Operating Model
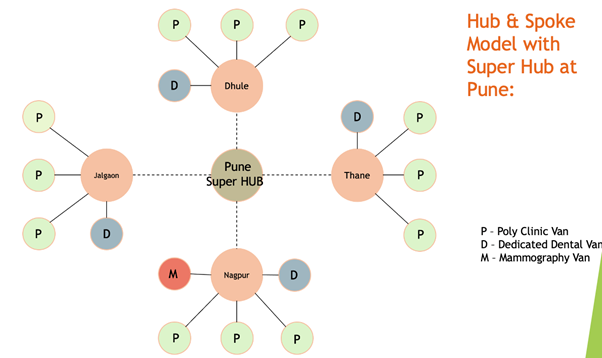
To begin with, we are going to have three types of Mobile Clinics as follows:
- Mobile Poly Clinics (Doctor + Dentist @Doorstep):- Majority of our clinics would be Poly Clinics with MBBS doctor and Dentist onboard with their teams.
- Dedicated Mobile Dental Van:- Some of our clinics would be dedicated dental vans which will look after elective and complex dental procedures identified and lined up by our Mobile Poly Clinics.
- Mammography Van (Pink Van):- Only in major cities – Breast & Cervix Cancer screening -(Mammography – every year after age of 45 American cancer society ).
Cost Overview of Mobile Poly Clinic:
- All OPD services (MBBS doctor & Dentist) and basic medicines will be free of cost for patients.
- Only dental procedures will be charged at no profit no loss basis.
- Per patient Cost for poly clinic is only Rs 154 (including dental checkups).
(1 Mobile Poly Clinic = 30,000 patients/Year)
Impact We Are Making
- Return on Investment (ROI)
- For every Rs 154 we are going to spent on each patient, ROI of Rs 4620 based on prevention service provided and emergency visits avoided. (Oriol et al BMC Central 2009 – ROI of $1:30 for Mobile Clinics).
- Additionally, we are saving patients from the pain, suffering and mental agony caused by advanced diseases.
- Ensuring right to Healthcare for underprivileged
- One prototype van of MBBS doctor and Dentist will visit around 30,000 patients annually breaching all access barriers.
- Quantifiable Objectives in every Healthcare Indicators such as Anaemia in Women, Child Health.
- Area specific and periodic targets for our field teams
- Non-Communicable diseases
- Diabetes, Hypertension, Heart Diseases, Stroke, Chronic Lung diseases (Responsible for 70% of all deaths worldwide-WHO).
- Committed to identifying at least 80% of undiagnosed cases of HTM & DM in a village.
- Capacity Building of local public health professionals like ASHA workers.
- Addressing healthcare infrastructure deficit
- Creation of durable healthcare infrastructure for local communities is vital for developing country like India.
- Saving for National Economy
- Timely diagnosis and treatment at doorstep will enhance productivity of workforce in terms of better wellbeing, less absenteeism due to illness.
Community Integration – how we work with them etc.
- Social Audit
- Apart from technological approach to ensure operational efficiency and discipline, continuous Social Audit will be undertaken. Outreach team will be constantly in touch with the village authorities and importantly our patients to take feedback.
- Expanding outreach with ASHA workers, local committees comprising of native influential individuals.









